We are at an increased risk of developing post-traumatic stress disorder (PTSD) following exposure to traumatic life events, including social victimization.[1]Autism Spectrum Disorder and Post-Traumatic Stress Disorder: An Unexplored Co-Occurrence of Conditions (Haruvi-Lamdan et al., 2020)
40% of autistics had PTSD symptoms during the last month, and over 60% experience PTSD at some point in their lives.[2]Experience of Trauma and PTSD Symptoms in Autistic Adults: Risk of PTSD Development Following DSM ‐5 and Non‐DSM ‐5 Traumatic Life Events (Rumball, Happé, & Grey, 2020)
Perceptions of trauma
Autistic people see and understand the world differently with a potentially unique perception of traumatic events. Intense anxiety responses to harmless situations, such as changes in routine or sensory stimuli, are common. Our traits create a heightened risk of post-traumatic stress disorder.[3]PTSD and Autism Spectrum Disorder: Co-morbidity, Gaps in Research, and Potential Shared Mechanism (Haruvi-Lamdan, Horesh, & Golan, 2017)[4]Experience of Trauma and PTSD Symptoms in Autistic Adults: Risk of PTSD Development Following DSM ‐5 and Non‐DSM ‐5 Traumatic Life Events (Rumball, Happé, & Grey, 2020)
Factors that make us more susceptible to PTSD:
- Autism increases the risk of exposure to traumatic events.[5]Autism Spectrum Disorder and Post-Traumatic Stress Disorder: An Unexplored Co-Occurrence of Conditions (Haruvi-Lamdan et al., 2020)
- Stress and trauma are a risk factor for comorbidity and the worsening of core autism symptoms, such as rigidity, rumination, and social withdrawal.[6]Autism Spectrum Disorder: The Impact of Stressful and Traumatic Life Events and Implications for Clinical Practice (Fuld, 2018)
- Shared mechanisms for PTSD and autism are our brain differences, as well as our thinking and behaviour.[7]PTSD and Autism Spectrum Disorder: Co-morbidity, Gaps in Research, and Potential Shared Mechanism (Haruvi-Lamdan, Horesh, & Golan, 2017)
- Lower intensity traumas may trigger PTSD symptoms in autistics who tend to have a heightened stress reactivity or altered perceptual experiences.[8]The Relationship Between Anxiety and Repetitive Behaviours in Autism Spectrum Disorder (Rodgers et al., 2012)
Criterion A
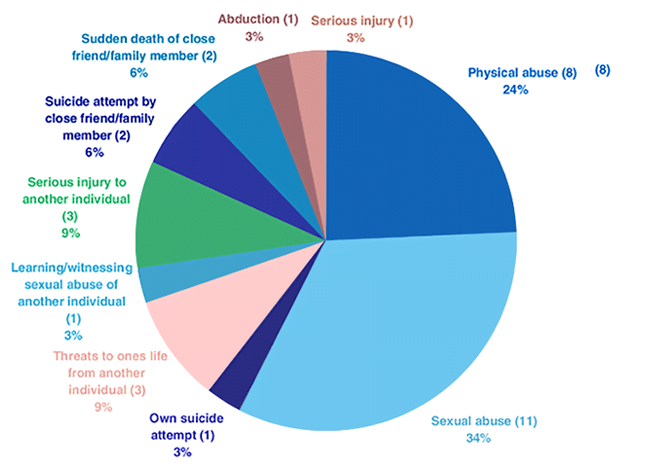
While a portion of our trauma fulfills the DSM-5 requirements, much of our PTSD is not recognized as trauma according to the DSM-5.
According to DSM-5 criteria, PTSD is only diagnosable if one of the four Criterion A events are met:
Criterion A
One required; The person was exposed to death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence, in the following way(s):
- Direct exposure
- Witnessing the trauma
- Learning that a relative or close friend was exposed to a trauma
- Indirect exposure to aversive details of the trauma, usually in the course of professional duties (e.g., first responders, medics)
Regardless of how stressful or severe events are, those not involving an immediate threat to life or physical injury such as psychosocial stressors (e.g., divorce, job loss, terminal cancer, and heart attacks) are not considered trauma by this definition. Yet patients who have experienced these issues regularly seek therapy or medications to deal with PTSD symptoms.
Social stressors
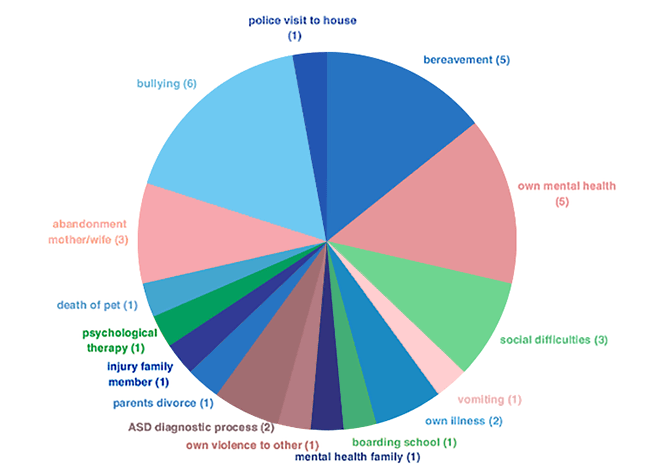
Autistics, especially females, reported more negative life events, particularly social events, than neurotypicals. 60% of autistics—but only 20% of neurotypicals—consider a social event as their most distressing experience.[11]Autism Spectrum Disorder and Post-Traumatic Stress Disorder: An Unexplored Co-Occurrence of Conditions (Haruvi-Lamdan et al., 2020)
Lots of trauma
Many events not included in the DSM criteria are known to trigger the development of PTSD. For example, the sudden unexpected death of a close relative or friend, or cumulative and prolonged stress from bullying or harassment.
8.5% experienced 1 trauma
10.2% experienced 2 traumas
13.6% experienced 3 traumas
20.3% experienced 4 traumas
10.2% experienced 5 traumas
11.9% experienced 6 traumas
6.8% experienced 7 traumas
5.1% experienced 8 traumas
1.7% experienced 9 traumas
1.7% experienced 10 traumas
1.7% experienced 15 traumas
Treat the person NOT the DSM
When clinicians assess trauma and recognize PTSD symptoms, it is important to consider possible non-DSM-5 traumas in autistics. PTSD diagnosis and treatment should not be withheld simply due to the atypicality of the traumatic event.
In addition, it is important for clinicians to be aware of symptoms that overlap between PTSD and autism, so as not to conflate the two diagnoses. In the criteria below, all symptoms shared between PTSD and autism are italicized.
Criterion B
One required; The traumatic event is persistently re-experienced, in the following way(s):
- Unwanted upsetting memories
- Emotional distress after exposure to traumatic reminders
- Physical reactivity after exposure to traumatic reminders
- Nightmares
- Flashbacks
Criterion C
One required; Avoidance of trauma-related stimuli after the trauma, in the following way(s):
- Trauma-related thoughts or feelings
- Trauma-related reminders
Criterion D
Two required; Negative thoughts or feelings that began or worsened after the trauma, in the following way(s):
- Overly negative thoughts and assumptions about oneself or the world
- Exaggerated blame of self or others for causing the trauma
- Negative affect
- Feeling isolated
- Difficulty experiencing positive affect
- Inability to recall key features of the trauma
- Decreased interest in activities
Criterion E
Two required; Trauma-related arousal and reactivity that began or worsened after the trauma, in the following way(s):
- Irritability or aggression
- Hypervigilance
- Heightened startle reaction
- Difficulty sleeping
- Risky or destructive behaviour
- Difficulty concentrating
Conclusion
PTSD in autistics is far more common than previously thought. The new DSM-5 criterion A misses people in an attempt to cast a smaller net. A narrowed definition does not negate PTSD but merely limits the assistance to those with PTSD. When non-A criteria cause PTSD, a person is considered not to have PTSD. Someone who qualified for PTSD in 2013, may no longer qualify.
Also important to consider is the diversity of what constitutes a trauma to an autistic versus a neurotypical. We know events that traumatize autistics are broader as opposed to neurotypicals. For example, there have been cases where filling out forms causes PTSD symptoms in autistic people.
A curiosity of mine is the significant overlap between autism and PTSD. I wonder, with such high numbers of us having PTSD, if symptoms that we think of as autism are, in fact, PTSD symptoms. Are the descriptions are so widely shared that we have come to think of them as autistic symptoms?
Read about why the autistic brain
is vulnerable to PTSD here:
Comments
Let us know what you think!