In my previous article on autism & sleep problems, I looked at the causes of sleep problems among autistic people. In this article, I will look at solutions.
Treatments for sleep problems
Autistic people show low levels of melatonin, making them prone to sleep disturbance. As such, they are sensitive to a lack of sleep hygiene.
Considering these (underlying) causes, sleep problems in autism can be improved or resolved by:
- Pharmacological treatment in the form of melatonin intake.
- Behavioral treatment with a focus on sleep hygiene.
Pharmacological treatment
Melatonin treatment has been proven to be successful in many cases where sleep hygiene intervention failed, showing improvements in total nighttime sleep and sleep latency (the length of time that it takes to accomplish the transition from full wakefulness to sleep) in children.[1]A randomized, placebo‐controlled trial of controlled release melatonin treatment of delayed sleep phase syndrome and impaired sleep maintenance in children with neurodevelopmental disabilities
Research from 2008
In a study from 2008, 170 autistic children were administered melatonin as treatment for insomnia. These were the findings based on parental reports:[2]Melatonin for Insomnia in Children With Autism Spectrum Disorders
- Parents of 27 children (25%) no longer reported sleep concerns at follow-up visits.
- Parents of 64 children (60%) reported improved sleep, although continued to have concerns regarding sleep.
- Parents of 14 children (13%) continued to report sleep problems as a major concern.
- Parents of 1 child (1%) reported the child having worse sleep after starting melatonin.
- Parents of 1 child (1%) reported the child having undetermined response.
That is a rate of improvement/success of 85%!
Adverse effects
Only 3 children (2%) had mild side-effects after starting melatonin, which included morning sleepiness and increased enuresis (involuntary urination).
So you will have to decide if you want to take melatonin and risk having to wear overnight diapers for adults. 2 out of every 100 autistic people!*
- I’m joking of course; the research is based on children, so the risk of enuresis does not (necessarily) apply to adults. So take that risk and let us know whether you stayed dry during the night.
Research from 2018
A double-blind study from 2018 looked at the long-term efficacy (the ability to produce a desired or intended result) and safety of pediatric-appropriate prolonged-release melatonin (PedPRM) with a sample of 95 children with ASD, and found the following after 52 weeks of continuous treatment:[3]Long-Term Efficacy and Safety of Pediatric Prolonged-Release Melatonin for Insomnia in Children with Autism Spectrum Disorder
- Subjects slept on average 62.08 minutes longer (with a standard error of 21.5 minutes).
- Subjects fell asleep 48.6 (10.2) minutes faster.
- Subjects had 89.1 (25.5) minutes longer uninterrupted sleep episodes.
- Subjects had 0.41 (0.12) less nightly awakenings (>50% decrease).
- Subjects had better sleep quality compared with baseline.
76% of the children that completed the treatment achieved overall improvement of ≥1 hour in total sleep time and sleep latency—or both—over baseline.
Adverse effects
Most frequent treatment-related adverse events were fatigue (5.3%) and mood swings (3.2%).
Behavioral treatments
Behavioral treatment tools to promote better quality sleep include:
- Bedtime pass — For children 3–10 years old it can help to create a “bedtime pass” that the child can use one time after bedtime, granting them access out of the bedroom for 5 minutes or less.[4]Steps in the use of the Bedtime Pass | Oregon Health & Science University This helps in establishing a bedtime routine and improves total nighttime sleep.
- Bedtime scheduling — For children it can help to schedule bedtime, with consist times for naps, night rest, and wake time. This entrains the circadian rhythm and reduces sleep debt.
- Bedtime routine — A bedtime routine can be particularly useful for autistic people—for children and adults alike—for the same reasons as bedtime scheduling.
- Chronotherapy — For individuals with delayed sleep phase disorder who generally cannot reset their circadian rhythm by moving their bedtime and rising time earlier, chronotherapy can be helpful, where an attempt is made to move bedtime and rising time later and later each day—around the clock—until the individual is sleeping on a normal schedule. This is quite a drastic method, however, and should thus be one of the last treatments to implicate when other treatments failed.
- Extinction — The extinction technique constitutes withdrawal of parental attention (for example petting the child on the back instead of taking them out of the crib or allowing them out of the bedroom),[5]Extinction Bursts and Your Baby’s Sleep | The Baby Sleep Site which can be a useful method in young children.[6]Treatment of infant sleep disturbance by trimeprazine in combination with extinction
- Faded bedtime — Bedtime fading is helpful for children (particularly 4+ years old) that are not sleepy at bedtime. It works by establishing a routine wake time and setting the bedtime about half an hour later initially. After following this schedule for three nights (while preventing the child from taking naps during the day), sleep latency will likely have reduced, at which point bedtime can be set earlier again.[7]What is “Bedtime Fading”? | Rosenberg Center This is likely to result in an increased amount of nighttime sleep, a decrease in night wakings, and a decrease in daytime sleep.[8]A faded bedtime with response cost protocol for treatment of multiple sleep problems in children
- Light therapy — Light therapy is effective for sleep problems in general, particularly for circadian outcomes and insomnia symptoms. However, most effect sizes are small to medium.[9]The effects of light therapy on sleep problems: A systematic review and meta-analysis
- Morning positive reinforcement — The child receives positive reinforcement for sleeping in their bed through the night. This treatment is used in combination with extinction; if the child attempts to sleep in another location, they are redirected back to their bed.
- Sleep hygiene — A set of rules and environmental improvements to promote better quality sleep, such as:
- Get up at the same time every day.
- The bedroom is free of noise.
- The bedroom is at a comfortable temperature.
- Eat regular meals.
- Don’t go to bed hungry.
- Avoid excessive liquids in the evenings.
- Cut down on all caffeine products.
- Enforcement of bed as a sleeping area only (sex is also fine, but only for adults).
- Avoid long naps.
- Exercise regularly.
It should also be noted—although it may be obvious—that promoting better sleep and longer nighttime sleep duration in your autistic child will in likely result in longer nighttime sleep for yourself as well.
So if you and your autistic child synchronize bedtimes, you can cut down sleep latency and enforce an incredibly efficient sleep regime.
Meta-analysis
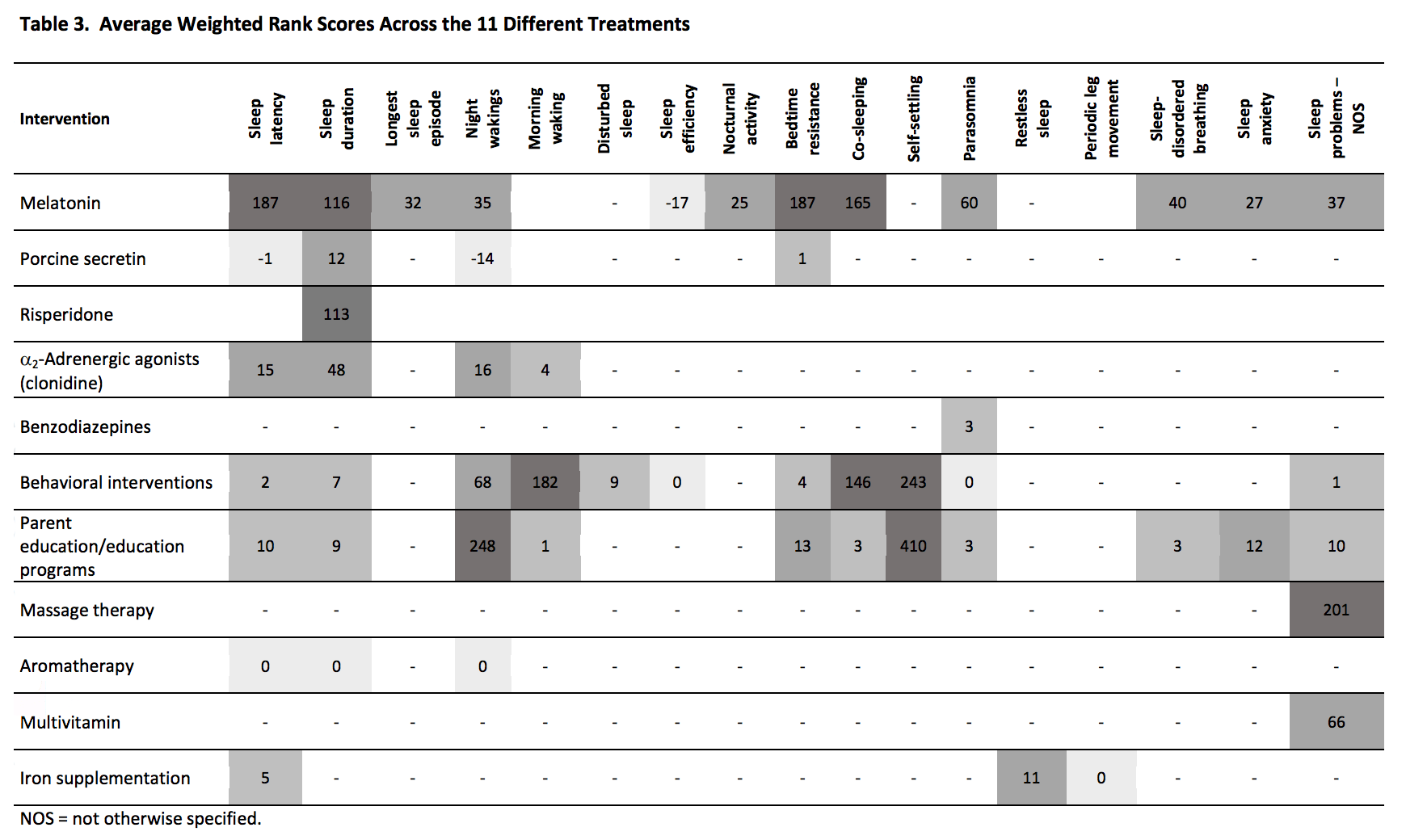
Based on a meta-analysis done in 2017 of 38 original studies on interventions across 17 sleep problem domains, it was found that no single intervention is effective across all sleep problems in autistic children.[10]Effectiveness of Sleep‐Based Interventions for Children with Autism Spectrum Disorder: A Meta‐Synthesis
However, melatonin, behavioral interventions, and parent education- or education program interventions appear the most effective at resolving sleep problems in multiple domains compared with other interventions.[11]Effectiveness of Sleep‐Based Interventions for Children with Autism Spectrum Disorder: A Meta‐Synthesis
Have a look at the table below for an overview of 11 treatments and their scores across the various sleep problem domains.
Improve your sleep hygiene
Considering sleep hygiene was found to be the predominant cause of sleep problems in autistic people—or I should say, autistic children—there are steps one can take to improve sleep hygiene, which may just resolve the sleep problems experienced.
Have a look at the illustration below for things you can focus on to improve your sheep hygiene.
PS: Don’t be too strict about any of these things and simply test
various approaches and stick with what works best for you!
Blue light-absorbing glasses
To help with sleep hygiene, it can be helpful to wear protective glasses that absorb blue light emitted by electronic devices with screens. Read the article below to learn more about how such glasses can help.
Comments
Let us know what you think!